Success reported with office-based DMEK
Article originally published on Healio, Nov. 16, 2021.
Office-based surgery exploded into the popular consciousness with the publication of the 2015 Kaiser study, reporting more than 21,000 cataract operations performed safely and effectively in clinic minor procedure rooms.
Since then, office-based surgery (OBS) suites have trickled into existence throughout the United States. These have primarily been designed for cataract surgery, but for the past year, we have also been performing OBS Descemet’s membrane endothelial keratoplasty.

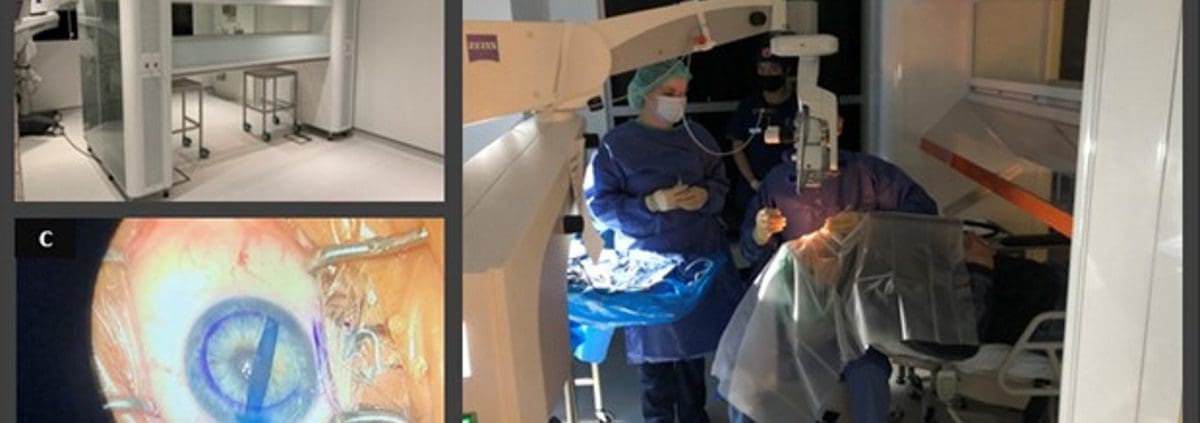
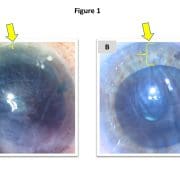
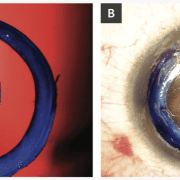
OBS DMEK offers several practical advantages. It is more convenient and comfortable to operate in clinic than in a hospital or even an ASC. It is also more cost-effective and more controlled because the supplies, the staff and the protocols are all determined by the surgeon. These features also tend to make the operation safer, particularly when combined with novel technologies designed to facilitate OBS procedures (the SurgiCube, for example, Figure 1).
OBS DMEK has therefore positively transformed our practice, but it has also required us to adopt new routines, including:
- 1) Topical anesthesia: At the Netherlands Institute for Innovative Ocular Surgery (NIIOS) in Holland, OBS DMEK has always been (and is still) performed using retrobulbar anesthesia. But in Birmingham, Alabama, we have switched to topical tetracaine (with no routine oral or IV anxiolytic). This has been well tolerated, although considering that DMEK is less invasive than routine cataract surgery, perhaps we should have expected this all along.
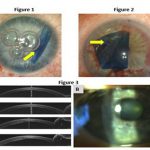
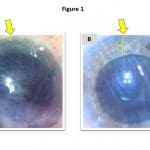
- 2) Descemetorhexis under air: Stripping Descemet’s membrane under air maximizes contrast and visibility. Maintaining an air fill of the anterior chamber is typically facilitated using an “air pump,” ie, an anterior chamber (AC) maintainer connected to a source of air infusion (most commonly, a vitrectomy machine). In OBS settings, however, such a machine is not likely to be available. Instead, the AC maintainer may be connected to a 60 cc syringe that is operated by a scrub tech/assistant, applying steady pressure to the plunger to maintain a gentle air flow.
- 3) Peripheral iridotomy creation: In a hospital setting, our preferred technique for peripheral iridotomy creation is via vitrectomy handpiece. But, again, with the unavailability of such a machine in an OBS setting, we have switched to using a YAG laser on the day of surgery, just before the operation. Fortunately, rates of pupillary block remain low with either technique.
- 4) No supine posturing: By far, this has been the biggest change to our practice. Conventionally, patients who undergo DMEK maintain supine posturing for 60 to 90 minutes postoperatively and are then discharged with instructions to remain supine for an additional 48 hours. Since switching to OBS DMEK, we have changed our protocol: Now, patients sit up immediately after surgery and proceed home without any positioning instructions. We are in the process of formally collecting our results of “no-supine DMEK” for academic publication, but so far, there does not appear to be any impact on detachment or re-bubbling rates.
OBS DMEK is not a new concept; it has been the “NIIOS standard” for close to 15 years with continued success. And here again, it looks like the world may be ready to follow the lead of Gerrit Melles into the future.

Leave a Reply
Want to join the discussion?Feel free to contribute!