Keratoconus
Keratoconus is a potentially serious eye problem usually diagnosed in young adults. The disease is characterized by progressive warpage of the cornea, the clear front surface of the eye. Over time, continued corneal warpage may produce a scarred and misshapen eye, which can permanently degrade the patient’s appearance and quality of vision.
What causes Keratoconus?
Chronic eye rubbing is strongly linked to keratoconus. Prior refractive surgery (including LASIK, PRK, and radial keratotomy or RK) may also trigger keratoconus, even many years after surgery. Keratoconus can also be inherited, so relatives of patients should be screened for the condition.
How is Keratoconus treated?
Keratoconus is a disease that progresses through stages. Initially, during the mild stages, the symptoms of keratoconus (especially blurred vision) may be improved with stronger glasses or contact lenses.
But as the disease progresses, glasses and ordinary contact lenses may lose their effectiveness, especially if the patient’s cornea ruptures or begins to scar. In these cases, corneal transplantation may be necessary to maintain or regain vision.
Until recently, it was not possible to halt the progression of keratoconus. But in 2017, the FDA approved a breakthrough new technology called UV-corneal-crosslinking which has a greater than 98% success rate at stopping keratoconus from worsening.
Corneal crosslinking has been widely regarded as one of the most significant modern advances in ophthalmology and among the most important innovations ever in the treatment of keratoconus.
What is UV-corneal crosslinking?
UV-corneal crosslinking is an FDA approved procedure for the treatment of progressive keratoconus. The procedure involves the administration of a specially formulated riboflavin solution to the corneal surface which is then activated by a UV-laser. This process tightly links the cornea’s fibers together, strengthening the cornea, and reducing the risk of continued disease progression.
What is the experience of corneal crosslinking like?
Corneal crosslinking is a routine procedure performed comfortably in our clinic. You are encouraged to eat a light meal beforehand, and to wear loose, comfortable clothing. An ophthalmic technician trained in corneal crosslinking will meet you on the day of your procedure and remain with you for the duration of the treatment, which takes approximately one hour. Most of this time is spent receiving riboflavin eye drops. Your corneal specialist will administer your UV laser treatment. This laser is painless and invisible. After your procedure, you are invited to enjoy a drink and a treat in our recovery area before going home.
Is corneal crosslinking covered by insurance? What if I don’t have insurance?
Corneal crosslinking is a covered procedure for the vast majority of medical insurances. If insurance coverage is unavailable, a variety of options exist for financing treatment.
Will corneal crosslinking improve my vision?
Corneal crosslinking will not undo the damage that has already been done. Therefore, it is important to be treated early, before significant damage to accumulates. To regain lost vision, additional procedures after crosslinking may be necessary.
What options do exist to improve my vision with Keratoconus?
Keratoconus causes visual loss through progressive warpage and scarring of the cornea. Several options exist to reverse or compensate for these problems, including:
- INTACS
- CAIRS
- Implantable collamer / contact lenses
- Corneal transplantation
Some, but not all, of these procedures are covered by most medical insurances. For non-covered procedures, financing options exist, which can be found here.
What are INTACS?
INTACS are acrylic segments which are inserted into the cornea to normalize the shape. These segments are typically implanted in the office, and most often result in a mild to modest improvement in vision, usually equal to 1-2 lines on the eye chart. Many, but not all, insurance plans cover the cost of INTACS implantation.
What are CAIRS
CAIRS are similar to INTACS, except that the implanted segments are made from human collagen, rather than acrylic. By using collagen, much more of the patient’s corneal warpage may be safely corrected, leading to potentially greater improvements in vision after surgery – usually 3-4 lines, or more. Some, but not all, insurance plans cover the cost of CAIRS implantation.
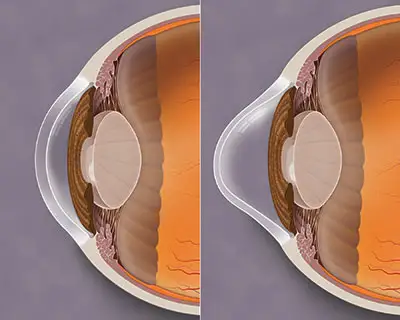
What are implantable collamer / contact lenses (ICLs)?
Implantable collamer lenes (also called implantable contact lenses) are soft lenses that may be placed inside the eye. This is a refractive procedure (like LASIK) which may take the place of glasses or soft contact lenses. ICLs take the place of strong glasses or soft contact lenses and may correct large amounts of near-sightedness and/ or astigmatism. Implanting these lenses is regarded as a minor procedure and is typically done in the office. Most insurance plans do not currently cover ICL implantation.
What is corneal transplantation?
Corneal transplantation is a procedure designed to replace part or all of the patient’s damaged cornea. This is typically regarded as the most aggressive option for treatment, and therefore, efforts are usually made to try less invasive alternatives, first.
A number of different types of corneal transplantation options exist for patients with keratoconus. These include Bowman layer transplantation, deep anterior lamellar keratoplasty, and penetrating keratoplasty, which differ according to how much of the cornea is transplanted.
Corneal transplantation may be performed in a minor procedure room in the office, or in a surgery center, depending on the patient and the anticipated complexity of the operation.
Most insurance plans cover the cost of corneal transplantation. In cases in in which insurance coverage is unavailable, the out-of-pocket cost varies according to the type of transplant performed.
Fuchs Dystrophy
What is Fuchs Dystrophy?
Dr. Jack Parker explains
Fuchs dystrophy is a problem that occurs within one of the five layers of the cornea – the endothelium. The endothelium is the inner lining of the cornea, and it’s made up of a single layer of microscopic pump cells, which function to keep the cornea thin and clear.
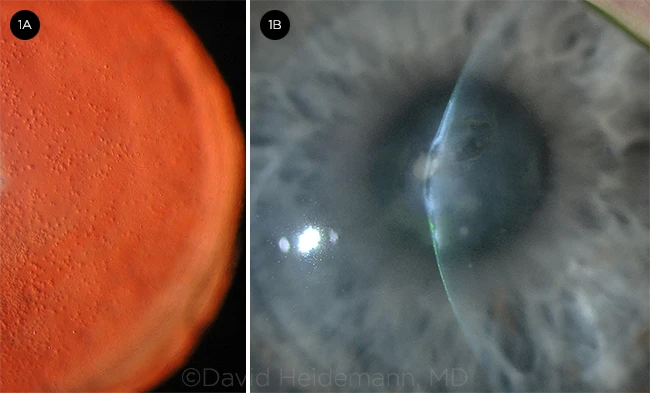
In patients with Fuchs dystrophy, this endothelial layer becomes dysfunctional, and the pump cells start to die. As a result, the entire cornea may become swollen and hazy. Eventually, fluid-filled blisters may appear on the surface of the cornea, and one or both eyes may turn grey. This process is typically associated with a gradual reduction in vision and, over time, can become painful.
What causes Fuchs Dystrophy?
No one knows the cause of Fuchs dystrophy, although the disease often runs in families, so the condition is probably at least partially genetic.
What are the symptoms of Fuchs Dystrophy?
Low quality vision is the first sign, along with increased difficulty with tasks that require high visual performance, for example driving at night or reading under poor illumination. The world may appear less vibrant or less vivid. Color vision is often affected, with things appearing grey or “washed out,” particularly as the disease advances. Eventually, late-stage Fuchs dystrophy includes all of these symptoms, along with ocular pain, as blisters begin to form on the corneal surface.
How is Fuchs Dystrophy treated?
Fuchs dystrophy is now effectively curable, thanks to modern advances in corneal surgery. Today, the endothelial layer of the cornea can be selectively replaced. There are two strategies to achieve this goal, represented by two different surgeries.
- DSAEK: This surgery was invented in 1998 in Holland and proved, for the first time, that it was technically possible to replace only the patient’s dysfunctional endothelium, without performing a full corneal transplant. Although this operation is now more than 20 years old, the procedure has a strong track record of success.
- DMEK: This surgery was invented in the 2000’s, specifically as a modern upgrade of DSAEK. It is specifically designed to be less invasive and to provide faster recovery, better vision, reduced need for postoperative eyedrops, and lower risk of complications.
DMEK is currently recognized as the superior surgical technique for most patients. However, in the United States, DSAEK is still more commonly performed by doctors, because DMEK is a much more technically difficult operation, for the surgeon. This is why it is critical for patients with Fuchs dystrophy to receive care at cornea specialty centers with a long history of success with DMEK, before proceeding with care.
What is Descemets stripping only (DSO) or Descemet membrane without endothelial keratoplasty (DWEK)?
For some patients with Fuchs dystrophy, it may be that the corneal endothelial layer is capable of some self-regeneration, and simply removing the dysfunctional areas (without supplying any new endothelial cells), can be enough to correct the problem of corneal clouding. This procedure, where only the dysfunctional cells are removed without supplying any new cells goes by several names including “Descemet stripping only” / “DSO” and “Descemet membrane without endothelial keratoplasty” / “DWEK.”
DSO and DWEK are still under investigation in the United States and abroad to determine who might be suitable candidates for this procedure.
DSO and DWEK are available for suitable candidates at Parker Cornea.
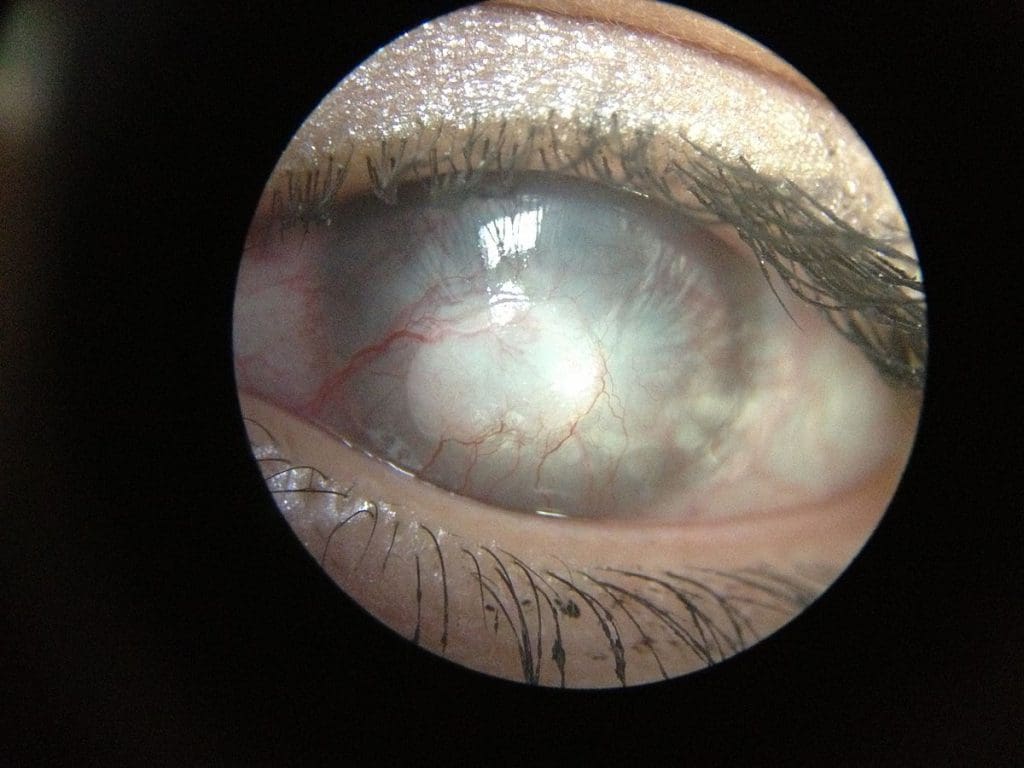
Bullous Keratopathy
Bullous keratopathy is a corneal disease with many different causes. The basic problem is failure of the cornea’s pump cell layer, causing corneal clouding, swelling, and the formation of painful fluid-filled blisters on the surface of the eye.
What causes Bullous Keratopathy?
Complicated prior surgery (especially cataract or glaucoma surgery) is the most common cause, followed by certain kinds of corneal infections.
How can I tell if I have Bullous Keratopathy?
If you’ve had complicated eye surgery, especially glaucoma surgery or cataract surgery, and now you have foggy or cloudy vision, worst in the morning, you may have the disease.
How is Bullous Keratopathy treated?
Bullous keratopathy is curable with surgery to replace the cornea’s failed endothelial pump layer. Frequently, eyes with bullous keratopathy also have other problems – with the iris, the lens, etc. Therefore, these may need to be fixed, as well, to prevent the bullous keratopathy from returning.
Corneal Scarring
What causes corneal scars?
Corneal scars may be the product of prior trauma, like injuries or infections, or they may arise as the result of certain disease processes, for example rare corneal dystrophies.
How do corneal scars affect my vision?
Corneal scars cause two basic problems – they undermine the clarity of the cornea, and they distort its shape. Normally, the cornea is an almost perfectly spherical, optically pristine instrument for projecting light into the eye, where it can be focused on the retina, so that images can be formed and passed to the brain.
Corneal scars, however, block the passage of light through the cornea. Furthermore, the light which does make it through the scar into the eye is typically distorted. As a result, the images formed on the retina are weak or washed out, rather than crisp and clear.
How are corneal scars treated?
This depends on the cause of the scar. Some can be treated through the use of a special type of hard contact lens, which does not remove the scar, but which may compensate for it.
Other scars must be removed. Mild scars can be eliminated by peeling them away, or through the use of a specialized laser. Others are so deeply embedded in the cornea that only a corneal transplant can effectively cure them.