Ring of trypan blue aids visualization in DMEK
When starting with Descemet’s membrane endothelial keratoplasty, it is common to manually mark a ring of purple dots on the corneal surface to serve as a centering guide for the graft’s final position.
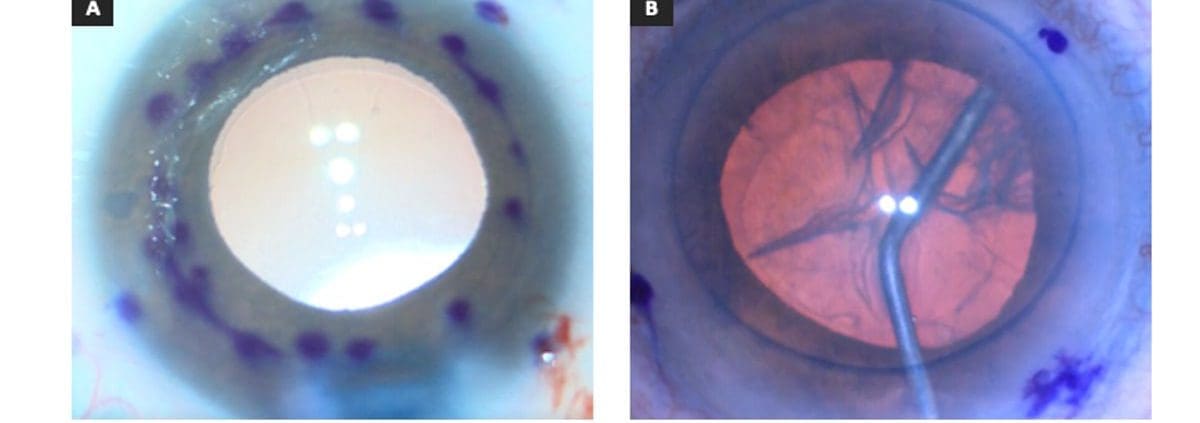
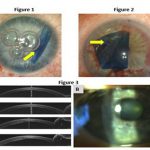
Although technically easy to apply, this array of purple dots may entail two notable drawbacks. First, inking the corneal surface is a somewhat tedious process and, while not inordinately time-consuming, nevertheless represents some period of extra manipulation. Second and more significantly, these purple dots may obscure the surgeon’s view of the most important part of the graft (its far edges), especially because ink marks are not easily applied precisely and may tend to bleed and run across the corneal surface (Figure 1a).

Source: Jack S. Parker, MD, PhD
As a result, while the purple dots may offer some benefit, they also involve extra effort and may worsen intraoperative visualization of the most important locations. Recently, we have discovered an alternative to the purple dots that is quicker and easier to apply and also avoids hindering the surgeon’s view of the underlying area.
Intraoperatively, after trephination of the graft to size, the same trephine is used to gently create a light circular impression on the recipient corneal epithelium. The cornea is then dried, and several drops of VisionBlue (trypan blue ophthalmic solution 0.06%, DORC International) are applied. This generates a vanishingly thin blue ring on the corneal surface, exactly the same size and shape as the graft (Figure 1b), which may serve as a useful landmark, both for stripping the recipient Descemet’s membrane and for centering the donor tissue.
Compared with the purple dots, the blue ring is more precise and more subtle. It is also less laborious to apply and less likely to interfere with visualization of the graft edges. As a result, it may permit better graft centration and easier identification of abnormalities at the graft edges, resulting in a theoretically reduced risk for detachment and improved postoperative outcomes.

Leave a Reply
Want to join the discussion?Feel free to contribute!