Short learning curve results in success with pinhole pupilloplasty
Article originally published on Healio, July 9, 2021.
Pinhole pupilloplasty has helped change many lives. The idea of small-aperture optics is not only simple but advantageous in cases of high astigmatism.
Jack S. Parker, MD, PhD, of Parker Cornea and the Netherlands Institute for Innovative Ocular Surgery (NIIOS), is my guest columnist this month, and he will explain with his co-author how to master pinhole pupilloplasty (PPP).
The terminology of pinhole pupilloplasty was suggested to me by David Chang, and I will always be grateful to him for coming up with such a suitable name. PPP can be done with any technique of iris suturing. Since McCannel started iris suturing and then Siepser took it to another level, so many others have pioneered in this area. Ogawa brought in the cerclage, and Ike Ahmed brought in the McAhmed suturing technique. Priya Narang helped pioneer single-pass four-throw pupilloplasty, for which I am indebted. The four-throw technique basically got us out of the locking system that was being used in all the iris suturing techniques. This made the whole surgery of iris suturing easy and possible by any surgeon. When we perform PPP, we generally use the single-pass four-throw pupilloplasty technique, although one can use any technique of their choice.
Pinhole pupilloplasty (PPP) was recently described for the treatment of severe corneal astigmatism. Pinhole apertures block stray distorted light rays and confer enhanced depth of focus. For this reason, pinhole IOLs are readily available in many places globally but not in the United States, where the FDA has yet to approve them. Therefore, Dr. Agarwal published a technique for recreating the pinhole aperture naturally by suturing the iris to produce a pinhole-sized pupil.
Initial publications with this technique are impressive: Eyes with more than 10 D and even more than 20 D of irregular (often fluctuating or unstable) astigmatism from prior penetrating keratoplasty or radial keratotomy are improved, in many cases achieving better than 20/40 (0.5) uncorrected vision. Further, PPP is cost-effective, uses already widely available and FDA-approved materials (suture), and is easily reversible without return to surgery, for example, by lasering the iris stitches, which can be done in clinic.
These advantages inspired us to start with PPP, and here, we describe some difficulties and insights acquired during our learning curve with the procedure.
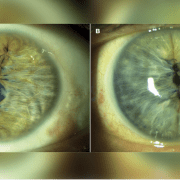
1. Size is important. Ideal for most patients is 1.5 mm. Any larger, and the benefit of the pinhole aperture is reduced (Figure 1a). If smaller, visual acuity can become limited by diffraction (Figure 1b). Consider erring on the side of “too small” because the pupil may be subsequently enlarged via YAG laser postoperatively.

2. Centration is important, too. The pinhole aperture should be fashioned around the first Purkinje image as a reference marker. A decentered pinhole-sized pupil is as optically offensive as a decentered multifocal IOL and reliably results in suboptimal visual outcomes (Figure 2).

3. Use bracketing sutures. Both sides of the pupil must be sutured. Otherwise, when the preoperative or intraoperative miotic agent wears off, the patient will experience asymmetrical re-dilation (Figure 3).

4. Suturing is facilitated by micro-grasping forceps. Dr. Agarwal originally described a “railroad technique” in which the suturing needle passes through the distal iris, a 26-gauge needle passes through the proximal iris, and the two are docked together and withdrawn from the eye. However, the 26-gauge needle often creates large needle track holes in the proximal iris, which are cosmetically and perhaps functionally detrimental (Figure 4a). So, we have replaced the 26-gauge needle with 25-gauge micro-grasping forceps, which may be used to hold and withdraw the suturing needle from the eye (Figure 4b). At present, Dr. Agarwal uses a 30-gauge needle, which is smaller and less traumatic to the iris.

5. Consider combining PPP with phacoemulsification and IOL implantation. Best for surgeons starting with PPP are phakic eyes also needing cataract surgery. In such cases, the phaco alone will likely render some benefit, obviating the need to execute the perfect PPP to satisfy patient expectations.
PPP has been a significant addition to our practice because, for the first time, we are able to offer some solution for patients with severe, irregular, fluctuating astigmatism (for example, from prior RK or PK) who are otherwise unable or unwilling to tolerate hard contact lenses. The procedure is quick and straightforward. It can be incorporated across most settings with ease as there is no need for specialized equipment.
Further, the operation is easy to recommend because, from their personal experience with eye exams, patients intuitively understand the visual improvement that they derive from pinholes. For doubters, a short course of topical pilocarpine may be tried preoperatively. Then, patients may be asked whether the resulting miosis improved their vision and, if so, whether they would like to have this effect recreated surgically.
PPP has predictable results that can be easily demonstrated preoperatively, allowing patients to have a tangible understanding and expectation of the procedure. It is also safe, reversible and highly effective for patients with few other options. After a short learning curve, it has become a regular surgical procedure at our practice, and most of our patients have reported great improvements without complications. As we continue to refine our technique, we expect even greater success with PPP.
- For more information:
- Jack S. Parker, MD, PhD, can be reached at Parker Cornea, 700 18th St. South, Suite 503, Birmingham, AL 35233; email: jack.parker@gmail.com.
- Edited by Amar Agarwal, MS, FRCS, FRCOphth, director of Dr. Agarwal’s Eye Hospital and Eye Research Centre. Agarwal is the author of several books published by SLACK Books, sister company of Healio publisher Ocular Surgery News, including Phaco Nightmares: Conquering Cataract Catastrophes, Bimanual Phaco: Mastering the Phakonit/MICS Technique, Dry Eye: A Practical Guide to Ocular Surface Disorders and Stem Cell Surgery and Presbyopia: A Surgical Textbook. He can be reached at 19 Cathedral Road, Chennai 600 086, India; email: aehl19c@gmail.com; website: www.dragarwal.com.